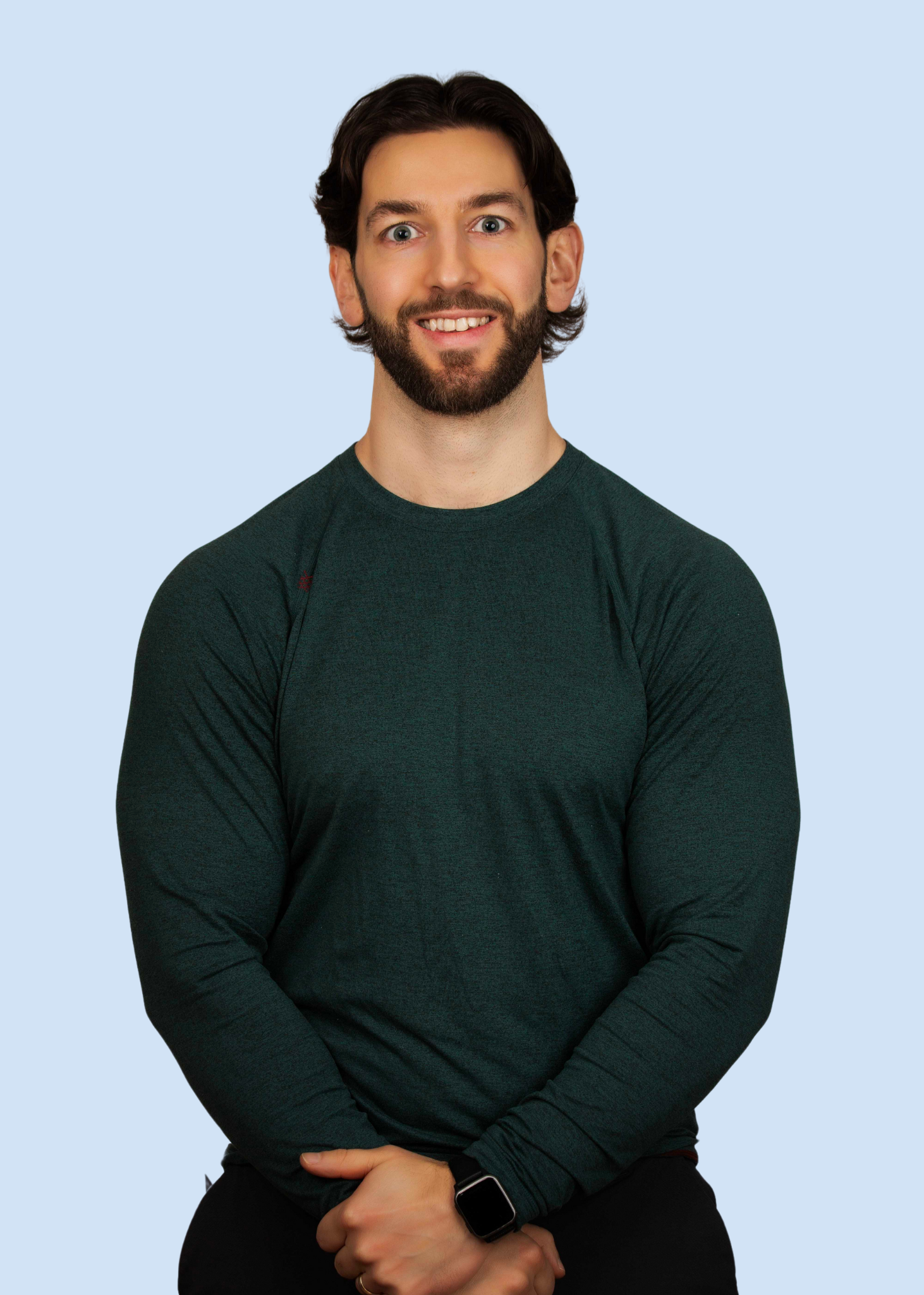
Your Partner in Pain-Free Living
I'm Jacob Perich, a passionate and dedicated physiotherapist committed to helping individuals overcome chronic pain and reclaim their lives. With years of experience and a deep understanding of the complexities of chronic pain management, I founded the Pacific Pain Centre with one goal in mind: to provide personalized care and effective treatment strategies to each of my clients.
My Journey
In September 2021, I embarked on a transformative journey following a series of three traumatic life events. Encountering debilitating pain accompanied by a myriad of perplexing symptoms, I sought answers from a variety of healthcare professionals over the course of three years, including doctors, neurologists, physiotherapists, massage therapists, naturopaths, pain specialists, psychologists, and counsellors. Despite receiving diverse diagnoses and conflicting treatment recommendations, my condition continued to deteriorate, leading to mounting frustrations and a deepening fear of movement and activity.
At my worst, I couldn’t walk for more than five minutes before the pain and numbness became unbearable. The activities that once brought me joy— running, hockey, lifting weights—were no longer options. Instead of excitement, they filled me with fear. Even the simplest daily tasks became a struggle, and just making it through the workday felt like an impossible challenge, day after day, for years. I couldn’t help but wonder, If this is me at 30, what does my future look like?
As my symptoms intensified, I shifted my perspective from associating symptom escalation with a worsening physical condition to understanding the role of sensitized tissue and a dysregulated nervous system in amplifying my pain experience. Embracing insights from Pain Reprocessing Therapy, pain neuroscience education, and mind-body medicine, I began to explore techniques aimed at regulating my nervous system and managing my chronic pain. This pivotal shift marked a turning point in my journey, offering newfound hope and empowerment in navigating the complexities of chronic pain management.
-
Lower back pain
Mid back pain
Neck pain
Left Anterior hip pain
Right posterior hip pain
Hamstring nerve tension
Quads nerve tension
Right knee pain
Left achilles pain
Right Shoulder pain
Right elbow pain
Left Leg numbness
Right foot numbness
Full body fasciculations/twitching
Hives/rashes
Skin mottling
Abdominal pain and
IBS
Headache
Fatigue
Blurred vision
Eye floaters
Frequently Sick
Conditions we treat
-
Nociplastic pain is a type of pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors, or evidence for disease or lesion of the somatosensory system causing the pain.
-
Neuroplastic pain refers to pain that arises from changes in the nervous system not due to physical injury or damage, but rather from the brain's ability to reorganize itself. This type of pain is often a result of neural pathways becoming sensitized or altered due to factors such as stress, trauma, or prolonged pain experiences. Unlike traditional pain that has a clear physical cause, neuroplastic pain is more about how the brain interprets and processes pain signals. Treatment often involves approaches like cognitive behavioral therapy, mindfulness, and other techniques aimed at retraining the brain and reducing the perceived pain.
-
Psychosomatic pain refers to physical pain that is influenced or exacerbated by psychological factors such as stress, anxiety, or depression. While the pain is real, its origin or intensity is linked to the mind-body connection rather than a purely physical cause. This type of pain can manifest in various forms, such as headaches, back pain, or stomach issues, and often requires a holistic approach to treatment, addressing both the physical symptoms and the underlying psychological factors.
-
Tension Myositis Syndrome (TMS), also known as Tension Myoneural Syndrome, is a term coined by Dr. John E.Sarno. It describes a psychosomatic condition where emotional stress and tension lead to physical symptoms, particularly chronic pain. Dr. Sarno believed that the brain distracts an individual from emotional issues by creating pain in the body, often in the back, neck, or limbs. The theory suggests that addressing the underlying emotional issues can alleviate the physical symptoms.
-
Mind-body pain refers to physical discomfort that is influenced by psychological factors. This type of pain often stems from stress, anxiety, depression, or emotional distress. The mind and body are interconnected, meaning mental states can manifest as physical symptoms.
Providing Services for
I support people living with ongoing or chronic pain—whether it's back pain, nerve pain, joint pain, fibromyalgia, or pain that hasn't had a clear diagnosis. If you're feeling stuck, frustrated, or unheard, you're not alone. I’m here to walk alongside you with a gentle, science-based approach that helps you make sense of your pain, reconnect with your body, and move toward the life you want to live—one step at a time
-
Often persists even after the initial injury has healed, due to the brain's pain pathways becoming sensitized.
-
Characterized by widespread musculoskeletal pain, often linked to changes in how the brain processes pain signals.
-
Chronic pain in muscles and fascia that can be perpetuated by neural circuit sensitization.
-
Chronic tension headaches can result from neural pathways reinforcing the sensation of pain.
-
Abdominal pain in IBS can be related to neural circuit dysfunction rather than direct gastrointestinal issues.
-
A chronic pain condition typically affecting a limb after injury, with pain persisting beyond normal healing.
-
Pain perceived in a limb that has been amputated, caused by the brain's neural circuits still processing signals from the missing limb.
-
Pain in the jaw and surrounding muscles can persist due to neural circuit sensitization.
-
Often involves neural dysregulation, leading to persistent pain in the pelvic region without an identifiable cause.
-
Often includes pain that may be linked to changes in neural processing.
-
While sometimes caused by direct nerve damage, it can also involve
neuroplastic changes leading to persistent pain. -
Characterized by severe facial pain due to dysfunction in the trigeminal
nerve, often related to changes in neural pathways. -
While primarily a sensory-motor disorder, it can also involve chronic pain due to neural dysregulation.
-
Similar to Complex Regional Pain Syndrome, highlighting chronic pain conditions that involve abnormal pain signaling.
-
Pain that remains long after surgical wounds have healed, often due to
changes in the nervous system. -
Persistent pain following a whiplash injury, even after the physical injury has healed.
Take the First Step to Better Health
Join us on your journey to optimal wellness. Our expert team is ready to provide personalized care and support tailored to your unique needs. Get started today and experience the difference!